Predictive scoring model for subungual melanoma in situ
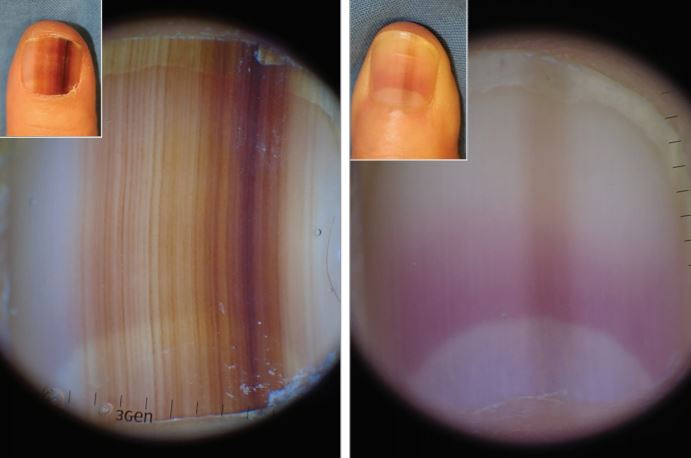
Can dermoscopy aid in the differentiation of subungual melanoma in situ from benign longitudinal melanonychia?
HealthCert Education
Can dermoscopy aid in the differentiation of subungual melanoma in situ from benign longitudinal melanonychia? A recent study investigated the characteristic dermoscopic findings of subungual melanoma in situ to establish a predictive scoring model for the diagnosis of the disease in patients with adult-onset longitudinal melanonychia affecting a single digit.
Subungual melanoma in situ is a malignant neoplasm that requires early diagnosis and complete surgical excision; however, little is known about the usefulness of the detailed dermoscopic features of longitudinal melanonychia to predict the diagnosis of subungual melanoma in situ.
A predictive scoring model for the detection of subungual melanoma in situ may assist clinicians in the examination of patients with adult-onset longitudinal melanonychia affecting a single digit.
In a study of 45 patients with pigmented nails, asymmetry, border fading, multi-colour pigmentation, width of the pigmentation of at least 3mm, and presence of the Hutchinson sign were features associated with subungual melanoma in situ. A predictive scoring model incorporating these features was reliable for the detection of subungual melanoma in situ, with a sensitivity of 89 per cent and a specificity of 62 per cent.
Of the total 45 patients with pigmented nails, the 19 patients with subungual melanoma in situ included 14 women and had an average age of 52 years, and the 26 patients with benign longitudinal melanonychia included 18 women and had an average age of 48.1 years.
Asymmetry (odds ratio [OR], 34.00; 95% CI, 3.88-297.70), border fading (OR, 9.33; 95% CI, 2.37-36.70), multi-colour (OR, 11.59; 95% CI, 2.21-60.89), width of the pigmentation of at least 3mm (OR, 5.31; 95% CI, 1.01-28.07), and presence of the Hutchinson sign (OR, 18.18; 95% CI, 2.02-163.52) were features of longitudinal melanonychia that were significantly associated with subungual melanoma in situ.
A predictive scoring model incorporating these dermoscopic features of subungual melanoma in situ was assessed. The model, ranging from 0 to 8 points, showed a reliable diagnostic value (the receiver operating characteristic curve had an area under the curve [C statistic] of 0.91) in differentiating subungual melanoma in situ from benign longitudinal melanonychia at a cutoff value of 3, with a sensitivity of 89 per cent and a specificity of 62 per cent.
This study suggests characteristic dermoscopic features for subungual melanoma in situ. A predictive scoring model based on these morphologic features may help differentiate the disease from benign longitudinal melanonychia.
Subungual melanoma has a poor prognosis compared to other types of melanoma mostly due to delay in diagnosis. This study concentrates on early features and so should help improve early diagnosis.
Source: Ohn J, Jo G, Cho Y, Sheu SL, Cho KH, Mun J. Assessment of a Predictive Scoring Model for Dermoscopy of Subungual Melanoma In Situ. JAMA Dermatol. 2018;154(8):890–896. doi:10.1001/jamadermatol.2018.1372
Learn more about skin cancer medicine in primary care at the next Skin Cancer Certificate Courses:


 1800 867 1390
1800 867 1390
.jpg)