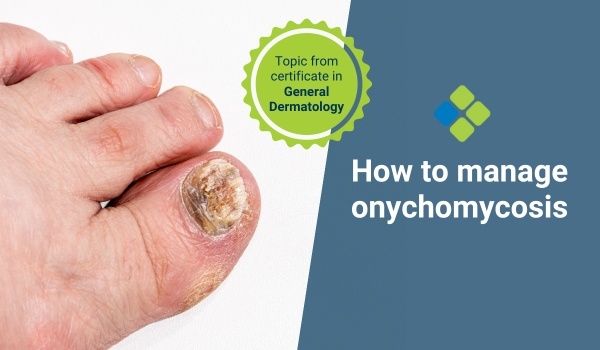
How to manage onychomycosis in primary care
Read a comprehensive approach to managing onychomycosis in primary care, including diagnosis, treatment, and preventive measures.
HealthCert Education
Onychomycosis, or nail fungus, affects millions worldwide. It is a common condition responsible for about 50 per cent of all nail disorders. Therefore, it is also a frequent presentation for GPs.
Onychomycosis is not life-threatening, but it can significantly impact a patient’s quality of life, leading to pain, discomfort, and social anxiety. Effective management within the primary care setting can help alleviate symptoms and improve patient outcomes.
What causes onychomycosis?
Onychomycosis is primarily caused by dermatophytes, a group of fungi that includes Trichophyton rubrum and Trichophyton mentagrophytes. However, non-dermatophyte molds and yeasts, like Candida species, can also be culprits.
Risk factors that contribute to the development of onychomycosis include:
- Age – The prevalence is higher in older adults due to slower nail growth and greater cumulative exposure to fungi.
- Comorbidities - Conditions like diabetes, psoriasis, and peripheral vascular disease increase susceptibility.
- Environment - Damp and communal environments, such as swimming pools or locker rooms, facilitate fungal transmission.
- Immunosuppression - Patients with compromised immune systems are more prone to infections.
Clinical presentation of onychomycosis
Onychomycosis can affect toenails, fingernails, or both. Common clinical presentations include:
- Distal Subungual Onychomycosis (DSO): The most prevalent form, characterised by nail thickening, discoloration, and subungual debris.
- White Superficial Onychomycosis (WSO): Presents as white, powdery patches on the nail surface.
- Proximal Subungual Onychomycosis (PSO): Often linked to immunosuppression, presenting with infection near the nail fold.
- Candida Onychomycosis: Often affects fingernails, particularly in individuals with chronic paronychia.
How to diagnose onychomycosis
When it comes to diagnosing onychomycosis, clinical examination alone may be insufficient. So, doctors need to consider the following diagnostic methods:
- KOH Preparation: A potassium hydroxide preparation can reveal fungal elements in nail clippings or scrapings.
- Culture: Fungal culture can identify the specific organism, although it may take several weeks.
- Histopathology: Nail biopsy can confirm diagnosis when other methods are inconclusive.
Onychomycosis management strategies
Managing onychomycosis in primary care involves a combination of:
- Patient education,
- Pharmacological treatments,
- Non-pharmacological interventions, and
- Preventive measures
Patient education
Educating patients on the nature of onychomycosis and emphasising that treatment can be prolonged and recurrence can occur is vital.
Pharmacological treatments
- Topical antifungals, such as Ciclopirox (Penlac), Efinaconazole (Jublia), and Tavaborole (Kerydin) for mild to moderate cases affecting less than 50 per cent of the nail plate.
- Oral antifungals, such as Terbinafine or Itraconazole, are suitable for more severe cases or when multiple nails are affected.
- Combination therapy with oral and topical treatments may also enhance efficacy, particularly in resistant cases.
Non-pharmacological interventions
- Laser therapy is a relatively new option that shows promise in improving nail appearance, though more research is needed to establish its efficacy.
- Surgical nail removal, followed by antifungal therapy, may be necessary in cases of severe pain or persistent infection.
Preventive measures
Advise patients to adopt preventive strategies to reduce the risk of reinfection:
- Keep nails clean, dry, and trimmed
- Wear breathable footwear and moisture-wicking socks
- Avoid walking barefoot in communal areas
- Use antifungal powders or sprays in shoes and on feet
Managing onychomycosis in primary care requires a comprehensive approach that combines accurate diagnosis, effective treatment, and preventive measures. By equipping patients with knowledge and resources, GPs can play a pivotal role in improving outcomes for individuals affected by this common yet challenging condition.
– Dr Rosmy De Barros
For further information on this topic, you may be interested to learn more about the HealthCert online Professional Diploma program in General Dermatology.
Engaging with this blog can help meet your annual
|

How to claim your CPD hoursIf you consume educational webinars, podcasts, articles, or research on this blog, you can Quick Log CPD hours with the RACGP via the usual self-submission process. You will be asked to reflect on what you have learned, and you will require supporting evidence such as a screenshot.Download the RACGP’s guide to self-recording your CPD here. |
Read another article like this one: How to manage liver spots
References
Leung, A. K., Lam, J. M., Leong, K. F., Hon, K. L., Barankin, B., Leung, A. A., & Wong, A. H. (2020). Onychomycosis: an updated review. Recent patents on inflammation & allergy drug discovery, 14(1), 32-45.
Gupta, A. K., MacLeod, M. A., & Tosti, A. (2018). Onychomycosis: clinical aspects. Scher and Daniel’s Nails: Diagnosis, Surgery, Therapy, 153-159.
Falotico, J. M., & Lipner, S. R. (2022). Updated perspectives on the diagnosis and management of onychomycosis. Clinical, Cosmetic and Investigational Dermatology, 1933-1957.
Gupta, A. K., Mays, R. R., Versteeg, S. G., Piraccini, B. M., Takwale, A., Shemer, A., ... & Tosti, A. (2019). Global perspectives for the management of onychomycosis. International journal of dermatology, 58(10), 1118-1129.

 1800 867 1390
1800 867 1390






