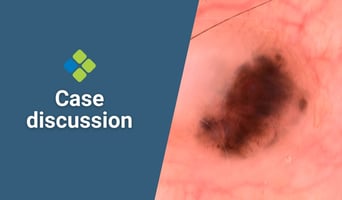
This week's case discussion, submitted by Dr Terry Harvey, features a 60-year-old male patient with...
Learn key nutrition assessment techniques and intervention strategies to provide more comprehensive healthcare.

This course explores the role of therapeutic diets in the treatment of chronic illnesses and nutritional disorders, highlighting the principles of the nutrition care process as applicable in a primary care setting.
- Tailored for medical professionals who wish to gain a better understanding of nutrition management.
- Teaches how medical nutrition strategies can be implemented to improve patient outcomes.
- This course is for medical doctors, International Medical Graduates, registered nurses, and degree-qualified health professionals.
- CPD-accredited and university-assured.
You might also be interested in the Primary Certificate of Medical Nutrition and Chronic Disease.
Fulfils 50 hrs for medical professionals in Australia*
100% online
$1595
Special rates available
94.5 hrs
Self-paced
*provided an outcome measurement activity with a minimum of 5 hours is completed.

- Learn about common dietary approaches, including Mediterranean, MIND, vegetarian, low GI, and more.
- Support your patients' weight management with effective communication and evidence-based strategies.
- Follow a weight-inclusive approach to healthcare to improve patient outcomes.
- Support patients with cardiovascular and GI conditions through tailored nutrition plans.
Get unlimited access to all course content, additional learning materials, ongoing post-course support, and more.
This module focuses on the role of nutrition and diet in the aetiology of major nutrition-related chronic diseases. Most chronic diseases are responsive to improved dietary choices. The dietary management of conditions including weight concern, coronary heart disease, hypertension, Type 2 diabetes mellitus, cancer and chronic kidney disease are outlined. Recognised dietary options such as plant-based diets, Mediterranean diet, DASH diet, vegetarian and MIND diet are discussed in detail. The course concludes with the discussion of isolated food groups and macronutrients in managing chronic disease including low glycaemic index (GI) food, low fat and high protein diets.
This module outlines the shift to weight-inclusive health care and recognises that both health behaviours and genetics may influence body weight. Weight classifications and limitations of BMI screening are discussed together with contributing chronic disease risk factors. A case study is presented to consider weight management dietary strategies including bariatric surgery, medication, nutrition and physical activity. Evidence based weight management strategies, potential risks of the diet culture, weight cycling and the relationship between dieting and mental health are discussed. A healthy lifestyle is preferable to a diet. People in bigger bodies may avoid medical care until conditions are advanced, to avoid weight bias and stigma. The non-diet approach looks at common assumptions in health care and the key principles of health at every size, including weight inclusivity, health enhancement, respectful care, eating for well-being and life-enhancing movement. The case study is revisited and options discussed including strategies to engage patients.
This module focuses on the role of diet in the prevention and treatment of common mental health disorders. The global burden of disease and the links to poor nutrition are discussed. Epidemiology and the role of nutrition in early life, adolescence and adulthood, links diet quality to brain and mental health outcomes. The gut-brain axis is explained including the relationship between mental health, gut health and gut microbiota. The content includes dietary interventions in the treatment of depression based on evidence from studies. Clinical practice guidelines are described. The key issues and barriers to improved diet and therefore improved mental health are discussed. A consistent multidisciplinary approach is required to facilitate best possible patient outcomes.
Eating disorders are serious mental health illnesses and can occur in any person, crossing boundaries of gender, age, culture and body size. In this module, diagnostic criteria for anorexia nervosa, bulimia nervosa, binge eating disorder, avoidance and restrictive feeding and intake disorder, and other specified feeding and eating disorders are listed. Understanding eating disorders including contributing factors are discussed. High risk populations, early identification signs and screening tools such as SCOFF and Eating Disorder Screen for Primary Care are outlined. The second section covers medical monitoring, inpatient admission criteria, treatment options and referral pathways including the dietician role. All patients with an eating disorder warrant initial medical monitoring to ensure safety, as eating disorders have the potential to negatively impact a wide range of physiological systems. Guides to medical monitoring criteria for inpatient admission and treatment options are explained including the role of the GP and the multidisciplinary team.
This module focuses on irritable bowel syndrome (IBS). It outlines the diagnosis, burden and pathophysiology of this condition including symptoms of food intolerances and the role of elimination diets as a treatment option. The mechanisms, clinical effectiveness, potential consequences and practical application of a low FODMAP diet are explained in detail. Guides on when to refer a patient to a dietitian are also outlined. The course concludes with a discussion on the role of diet and gut microbiota in the aetiology of gut conditions, including focusing on the microbiota in IBS.
This module examines the principles of motivational interviewing to guide health behavioural changes. The content includes recognising what triggers can lead to health behavioural change, discusses the challenges to patient’s engaging in change, and suggests various clinical tools to assist with this process. Change strategies including desire, ability, reasons and need, commitment strength measures, sustainability and change talk components are outlined. Four core skills of open questions, affirmations, reflections and summaries whilst practicing advanced listening skills can awaken motivation to change. The content then identifies and offers guidelines to work with resistance and discord and suggests ways to respond to change resistance and guide healthier outcomes.
This module focuses on the key nutritional problems for patients with diabetes and discusses healthy eating, defines carbohydrates, examines the glycaemic index vs glycaemic load, and includes the nutrition priorities for people with diabetes. The goals of diabetes management include healthy eating to positively influence glycaemic control, blood pressure, hyperlipidaemia and overweight/obesity. A healthy diet, physical activity and in some cases, pharmacological intervention contribute to glycaemic control. Carbohydrates (CHOs) are mentioned before moving to explaining the glycaemic index (GI) and its role in diabetes management. Nutritional priorities are discussed including weight loss, healthy eating and individualised plans. Low carbohydrate diets are defined including their relationship with GI and managing diabetes. The benefits and disadvantages of a low CHO/ketogenic diet in relation to managing diabetes are discussed. A case study reinforces course content.
GPs play an important role in directing patients with cardiovascular disease (CVD) to evidence-based nutrition advice and resources. This module discusses the evolution of evidence and heart health nutrition recommendations including the National Heart Foundation Eating for Heart Health Position Statement and other recent cardiovascular disease management and heart failure guidelines. Nutrient supplements are discussed together with cardiovascular nutrition controversies including food trends and omega-3, anti-inflammatory dietary components, and weight management. The second section discusses the key principles and evidence for the DASH and Mediterranean diets supported by evidence-based research. Guides are provided for the GP and the patient approach including patients with lower health literacy.
This module introduces the key nutritional considerations for patients with chronic and end stage kidney disease. It gives a broad understanding of the difference in nutrient recommendations and diet quality and identifies what presenting symptoms and issues in kidney disease can lead to further discussions about nutrition. The first section outlines nutrition problems in CKD patients stages 1-5 including chronic diseases such as CVD/diabetes/insulin resistance and/or malnutrition. The second section outlines the complexities of chronic kidney disease including kidney stones, hydration and electrolyte/fluid imbalance. The role of high and low potassium foods, vitamins and trace elements in improving patient outcomes is discussed. The content includes diagrams, guides, case studies and research.
If you're not interested in pursuing a full certificate in this field but simply want to enhance your skills in specific topics covered in this course, you can access the content of this and other courses for a flat fee of $83 per month (paid annually) within HealthCert 365.

Senior Research Fellow, Griffith University
Early Career Fellow, NHMRC
Associate Editor, Australian Journal of Primary Health
Executive Committee Member, Australasian Association for Academics in Primary Care
Dr Lauren Ball’s vision is that all Australians are supported by a health care system that allows them to reach their full potential in life. This will be achieved by making nutrition a prominent part of the ongoing care they receive in general practice – the first point of contact with the health care system.
Lauren has worked with community members, health professionals, education providers and professional bodies to conduct research on how patients can be better supported in general practice to eat well. She implements interventions and programs so that general practitioners, nurses, dietitians, nutritionists, pharmacists and other health professionals feel confident in nutrition and have the skills to best meet patients' needs. She also works with Primary Health Networks to better understand how primary care services can be reoriented to put nutrition and other lifestyle behaviours at the forefront of the health care system.
Lauren has published over 100 peer-reviewed scientific articles and attracted over $1 million in research funding from government bodies, non-government organisations and philanthropic foundations. She is a Senior Research Fellow at Griffith University and an NHMRC Early Career Fellow. She is also an Associate Editor for the Australian Journal of Primary Health and Executive Committee Member of the Australasian Association for Academics in Primary Care.

Dr Jaimon Kelly is an Accredited Practicing Dietitian and Senior Teaching Fellow at Bond University. Jaimon works in private practice and consults primarily for chronic disease nutrition. He is also an early career researcher passionate about improving patient-centred care in chronic disease, is an advocate for patient-engagement in both the clinical and research setting, and has a strong interest in exploring new ways to deliver dietary education to improve people’s dietary self-management.

Post-doctoral researcher, Princess Alexandra Hospital (PAH), Brisbane
Dr Hannah Mayr is an Accredited Practicing Dietitian who recently completed her PhD thesis at La Trobe University. Under the principal supervision of leading Mediterranean diet researcher, Prof Catherine Itsiopoulos, she investigated the effect of a Mediterranean versus low-fat diet on inflammation and adiposity in patients with coronary heart disease.
Hannah has published a number of reviews, methods and results-based papers within this work and received the ‘New Researcher Award’ at the 2018 Dietitians Association of Australia National Conference for her thesis work exploring a novel dietary assessment tool, the Dietary Inflammatory Index. Her research and practice interests are in dietary patterns and interventions, chronic disease and metabolic health.
Hannah currently works as a post-doctoral researcher at Princess Alexandra Hospital (PAH) in Brisbane and externally with La Trobe, which includes activities to enable implementation of the Mediterranean diet into routine care for chronic disease management. At PAH she leads a mentorship group focused on research capacity building for clinical dietitians. She also teaches into the Master of Nutrition and Dietetics at Bond University and she is passionate about engaging dietetics students in research activities.

Head of Translational and Educational stream, Food & Mood Centre, Deakin University
Dr Tetyana Rocks is a postdoctoral research fellow and Head of Translational and Educational stream at the Food & Mood Centre, Deakin University. Her main role within the centre is to support the translation of the current evidence in the field of Nutritional Psychiatry into policy and clinical practice through education and training of health professionals and the wider community in Australia and internationally. Tetyana is also continuing to developing her research in eating disorders, focusing on the role of gut microbiota in treatment. Tetyana is an Accredited Practicing Dietitian with extensive experience in tertiary education.

Dietitian & Postdoctoral Researcher, Food and Mood Centre, Deakin University
Dr Heidi Staudacher is a dietitian and postdoctoral researcher at the Food and Mood Centre at Deakin University. Her chief research interests include the pathophysiology and dietary management of functional gastrointestinal and mental health disorders, and the interaction of diet with the microbiome in these disorders.
Heidi was a NIHR Clinical Doctoral Fellow at King’s College London between 2012-2016 and during her PhD conducted a large randomised controlled trial investigating the effect of a low FODMAP diet with probiotic co-administration on the gastrointestinal microbiota, symptoms, dietary intake and quality of life. She has published several key papers in the field of dietary management of irritable bowel syndrome.

Clinical Psychologist, Psychology Consultants Pty Ltd
Adjunct Associate Professor, School of Psychology, The University of Queensland
Co-director, UQ Compassionate Mind Research Group
Dr Stan Steindl has over 20 years’ experience as a therapist, supervisor and trainer, especially providing training in Motivational Interviewing (MI). His PhD examined the use of MI with combat-related posttraumatic stress disorder and comorbid alcohol dependency, and he continues to work in the areas of trauma, addiction and health behaviour change, as well as having a general clinical practice. He is an active member of the Motivational Interviewing Network of Trainers (MINT), and delivers training in an engaging, informative and practical way.

Accredited Sports Dietitian
Treasurer, Australian & New Zealand Academy for Eating Disorders
Founder, River Oak Health
Founder, Food Mind Body
Shane Jeffrey is an Accredited Practicing Dietitian and Accredited Sports Dietitian with 25 years of experience as a dietitian in both the private and public sectors, working almost exclusively in the field of eating disorders, the non-diet approach and sports nutrition. Shane is the current treasurer and a past executive member of the Australian & New Zealand Academy for Eating Disorders, a past chairperson for the nutrition interest group for the Academy for Eating Disorders, and a past chairperson for the Eating Disorder Interest Group for the Dietitians Association of Australia.
Shane has a passion for supporting the education of health professionals in the eating disorders, teaching into four universities, facilitating workshops, and presenting at various national and international conferences. Shane is the founder of River Oak Health and Food Mind Body, two Queensland-based private practices dedicated to the treatment of eating, weight and body image concerns.

Senior Teaching Fellow and Internships Lead, Master of Nutrition and Dietetic Practice Program, Bond University
Christina Turner is an Accredited Practising Dietitian with almost 19 years’ experience working across a variety of settings including acute dietetics, community outpatients, public health and community development. More recently she has specialised in eating disorders and established SOL nutrition, a non-diet private practice in northern New South Wales, Australia.
Christina is currently a Senior Teaching Fellow and Internships Lead within the Master of Nutrition and Dietetic Practice Program at Bond University. She teaches into the clinical and communication/counselling subjects including eating disorders, weight-inclusive practice and non-diet nutrition, cognitive-behavioural therapy and motivational interviewing topics.

Study at your own pace and to your own schedule. Interactivity, discussion, and feedback opportunities are included.

Easily meet your CPD requirements and gain valuable skills – all in one place for $83 per month.
$1595
*provided an outcome measurement activity with a minimum of 5 hours is completed.
Bundle two courses and save 5%, or three courses and save 10% upon enrolment.
Talk to us about deferred payment options, registrar scholarships and special rates.


This is the pathway to improve your confidence and evolve into the GP you aspire to be.
Dr S. Shinwari
HealthCert courses have become the standard by which you gauge all others.
Dr K. Abolarinwa
Good, courses with excellent speakers. I particularly enjoyed the case study scenarios which helped to integrate the knowledge gained.
Dr A. Tucker
This is the pathway to improve your confidence and evolve into the GP you aspire to be.
Dr S. Shinwari
HealthCert courses have become the standard by which you gauge all others.
Dr K. Abolarinwa
| RACGP Activity Number | ACRRM Activity Number | Activity Title | Education Hours | Performance Hours | Outcome Hours | ||
|---|---|---|---|---|---|---|---|
| 482811 | 31258 | Latest trends in cardiovascular nutrition | 482811 | 31258 | 5 | 6 | 0 |
| 480526 | 31250 | Nutrition in gastrointestinal health | 480526 | 31250 | 4.5 | 6 | 0 |
| 480507 | 31247 | Chronic disease and diets: Med, MIND, vegetarian, high protein, low GI | 480507 | 31247 | 4.5 | 6 | 0 |
| 485087 | 31264 | Nutrition in chronic kidney disease | 485087 | 31264 | 4.5 | 6 | 0 |
| 482800 | 31257 | Are carbs the enemy? Understanding nutritional needs for patients with diabetes | 482800 | 31257 | 4 | 6 | 0 |
| 485477 | 31267 | Motivational behaviour change | 485477 | 31267 | 4.5 | 6 | 0 |
| 485074 | 31262 | Diet and depression | 485074 | 31262 | 4.5 | 6 | 0 |
| 485082 | 31263 | Eating disorders including anorexia and bulimia | 485082 | 31263 | 4.5 | 6 | 0 |
| 482250 | 31255 | Patient-centred weight management: Non-diet approach | 482250 | 31255 | 4.5 | 6 | 0 |
| 859573 | 33472 | Dietary and malnutrition for the management of chronic disease Outcome Improvement Activity | 859573 | 33472 | 0 | 0 | 8.5 |
| Total hours | 40.5 | 54 | 8.5 | ||||
View the CPD Hours for all HealthCert Education activities.
The purpose of outcome measurement activities is to improve your clinical confidence in managing an identified learning gap. Outcome measurement activities are not a requirement of our Professional Certificate of Advanced Certificate courses; they are a requirement for Australian CPD purposes.
HealthCert Education provides a variety of outcome measurements activities to suit your needs:
The Advanced Certificate of Clinical Nutrition is tailored for medical practitioners who wish to gain a better understanding of nutrition management in order to improve patient outcomes, especially for those patients with conditions commonly seen in general practice.
The course is suitable for medical doctors, degree-qualified health professionals, and International Medical Graduates. Participants must have successfully completed the HealthCert Professional Certificate of Clinical Nutrition course (or a qualification deemed equivalent).
Participants do not have to pass an IELTS test but, as the courses are delivered in English, proficiency in listening, reading and writing English is assumed.
Participants will require access to a computer/laptop, an internet connection and a basic level of technology proficiency to access and navigate the online learning portal.
Professionally recognised qualifications and prior studies may be recognised for entry into this course if the learning outcomes match exactly. Please ask a HealthCert Education Advisor for an individual assessment of your prior qualifications and experience.
This certificate course meets the minimum 50 hours CPD annual requirement across all three mandatory CPD activity types, provided an outcome measurement activity with a minimum of five hours is completed. You may use an optional HealthCert outcome measurement activity or develop your own.
Outcome measurement activities are not a requirement of Professional or Advanced Certificates.
Upon successful completion of the course requirements, course participants will receive the Advanced Certificate of Clinical Nutrition and CPD hours.
This certificate course:
To learn more about the delivery of certificates in Australia and overseas, please visit our FAQs.
Certificate Pathway
This course is the second stage of the two-part Certificate Courses in Clinical Nutrition. The education pathway is Professional Certificate of Clinical Nutrition and Advanced Certificate of Clinical Nutrition.
You might also be interested in the Primary Certificate of Medical Nutrition & Chronic Disease.
This organisation is an RACGP-accredited CPD provider under the RACGP CPD Program.





Don't see your question? Explore other faqs or talk to us.
Fees will vary based on the program and study option selected (fully online vs online + optional practical workshop). Payments can be made upfront or in monthly instalments. Special rates and various payment options are available. GP registrars and doctors in training enjoy a scholarship of up to $500. Talk to us to learn more.
Completion of any HealthCert course or attendance at an event will enable you to access the HealthCert Alumni Program which includes:
HealthCert Education is pleased to issue digital credentials for alumni. Digital credentials are a permanent online record of your successful completion of a HealthCert course and are issued to all course participants in addition to PDF certificates. If you are based in Australia, you also have the option to order a hard copy of your digital certificate for a small additional fee.
The recommended study duration of this certificate course is 94.5 hours, which includes study of the pre-course activities and readings, online lectures, live tutorials, and online assessment. This self-paced course offers the flexibility of 100% online study in your own time, at your own pace, in your own home or office, with no mandatory face-to-face requirements. You are not required to be online at specific times but can view and replay video lectures at your convenience.
All HealthCert courses meet World Federation of Medical Education standards. This certificate course qualifies for CPD hours from the Royal Australian College of General Practitioners (RACGP) and the Australian College of Rural and Remote Medicine (ACRRM) in Australia. It is recognised by the Royal New Zealand College of General Practitioners (RNZCGP) in New Zealand. It is recognised by the Hong Kong College of Family Physicians (HKCFP) in China. It is a self-submitted activity in Dubai and the United Kingdom. It is a self-submitted activity through the College of Family Physicians in Canada. If you live or work outside one of the above-mentioned countries, please contact us on admin@healthcert.com to discuss whether this course can be recognised in your country.
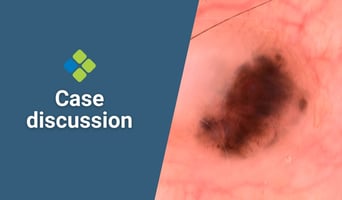
This week's case discussion, submitted by Dr Terry Harvey, features a 60-year-old male patient with...

"It is better to be a master of a couple of flaps rather than knowing a little bit about all the...

Severe sunburn is common, particularly during the summer months. While mild sunburn can often be...
Want to stay up-to-date with the latest case studies, podcasts, free video tutorials and medical research articles pertinent to primary care?
Our Education Advisors can assist you with any queries and tailor our education pathway to suit your current expertise, interests and career goals.